Medical tourism articles
Medical tourism articles, blog
22.03.2024
Georgia is one of the few countries in Europe where surrogacy is legal and regulated by law.
Benefits
Advantages of the surrogacy programme in Georgia:...
09.04.2024
Surrogacy in Europe is legal in the following countries:
Country
Access to surrogacy
Participation of foreigners in the program
Comme...
24.03.2024
As of 2024, there are three ways to get to Ukraine: by train, by bus, and by car.
As of February 24, 2022, air traffic with Ukraine has been temporarily susp...
09.04.2024
Oocyte donation, also sometimes referred to as egg donation, is a great way to help couples who are having fertility problems.
Oocyte donation – is the...
09.04.2024
Information for couples
If you are a couple and want to find a surrogate, we recommend you to contact a qualified clinic in Ukraine.
This will guarantee...
27.12.2023
Medical abortion – is one option for ending a pregnancy that can be chosen according to your personal circumstances and decisions.
We understand that m...
02.05.2023
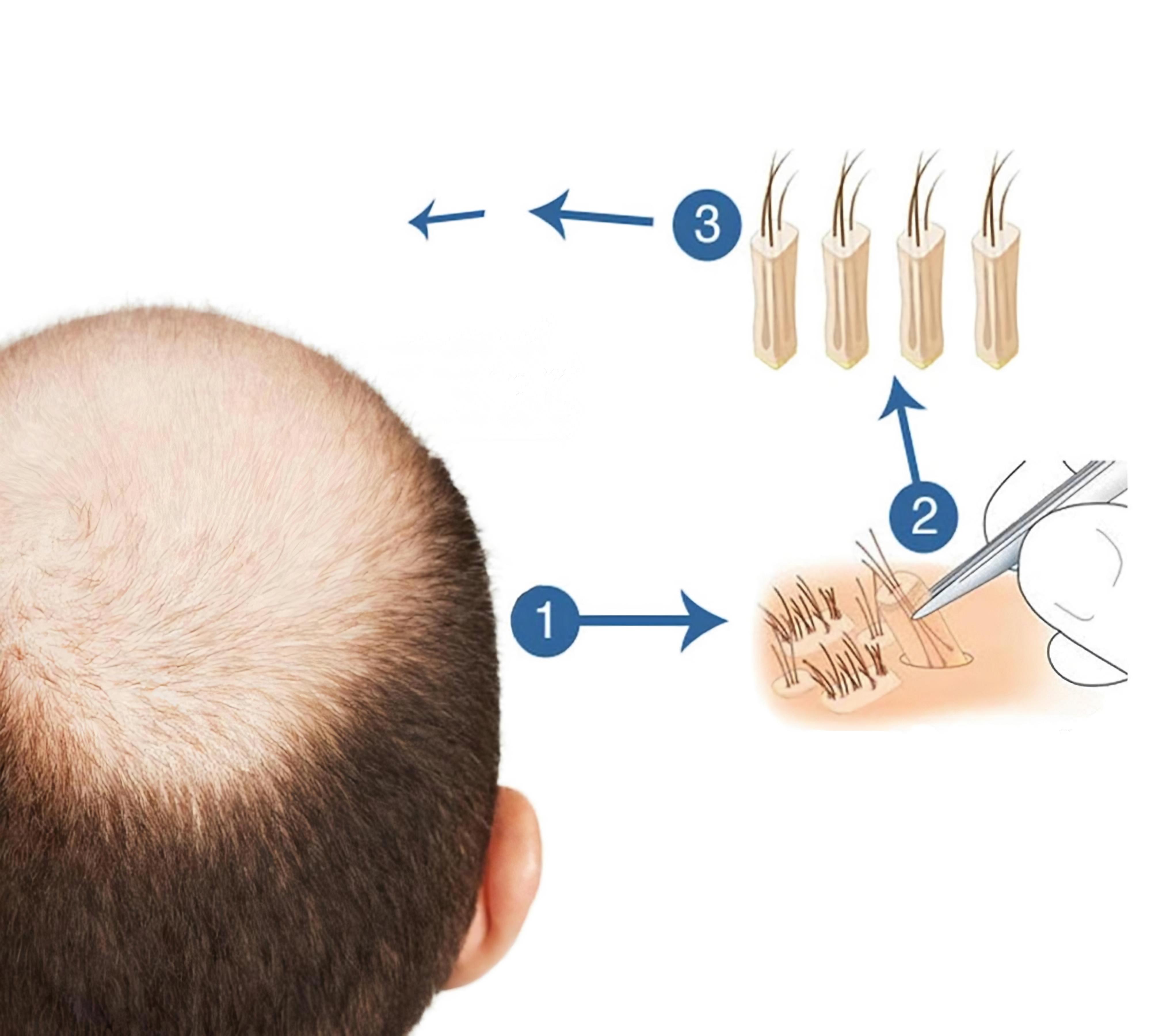
Embarking on a hair transplantation journey in Turkey can be both exciting and nerve-wracking. As a top destination for affordable and high-quality hair transpl...
28.12.2023
One of the pressing problems of humanity is the gradual decline in the general health of our population, which leads to the emergence of new problems, as well a...
13.01.2024
Masturbation is often cited as the cause of all mankind's ills, from health problems to declining birth rates. For example, a popular question on the forum...
15.04.2024
Hair transplantation is one of the most popular cosmetic surgery procedures. According to the International Society of Hair Restoration Surgery (ISHRS), about 1...
15.08.2022
History of Ukraine
Travelers have always been and, understandably, that to last on a horse or in a carriage for a long time, the whole and very prob...
02.08.2022
For the first time since 2012, the World Health Organization (WHO) has developed and released a new compendium of guidelines on abortion procedures and accessib...