Pancreatitis is an inflammatory disease of the pancreas, with manifestations in the form of irreversible changes in the structure of the organ, which cause pain and a steady decline in its function.
The pancreas performs important functions:
- the secretion of most digestive enzymes
- production of insulin (a hormone, insufficiency of which leads to diabetes)
There is a worldwide trend toward an increasing incidence of acute and chronic pancreatitis, more than doubling over the past 30 years.
Causes of pancreatitis
The most common cause of chronic pancreatitis is the consumption of alcohol, and the quality and raw material from which the drink is made do not matter.
Other reasons
- Toxins and metabolic factors:
- alcohol abuse
- smoking
- increased calcium content in blood (develops in patients with a tumor of parathyroid glands)
- Overeating and eating fatty foods
- Protein deficiency in the diet
- the effects of medications and toxins
- chronic renal failure
- Obstruction of the pancreatic duct:
- stones in this channel
- due to a malfunction of the sphincter of Oddi
- blockage of the duct by a tumor, cysts
- post-traumatic scarring of pancreatic ducts (complication of endoscopic procedures: papillosphincterotomy, stone removal, etc.)
- Pathology of the gallbladder and biliary tract.
- Pathology of the duodenum.
- Consequence of acute pancreatitis.
- Autoimmune mechanisms.
- Heredity (gene mutations, 1-antitrypsin deficiency, etc.).
- Helminths.
- Insufficient oxygen supply to the pancreas due to atherosclerosis of the vessels that supply blood to this organ.
- Congenital anomalies in the development of the pancreas.
- Idiopathic chronic pancreatitis (the cause cannot be determined).
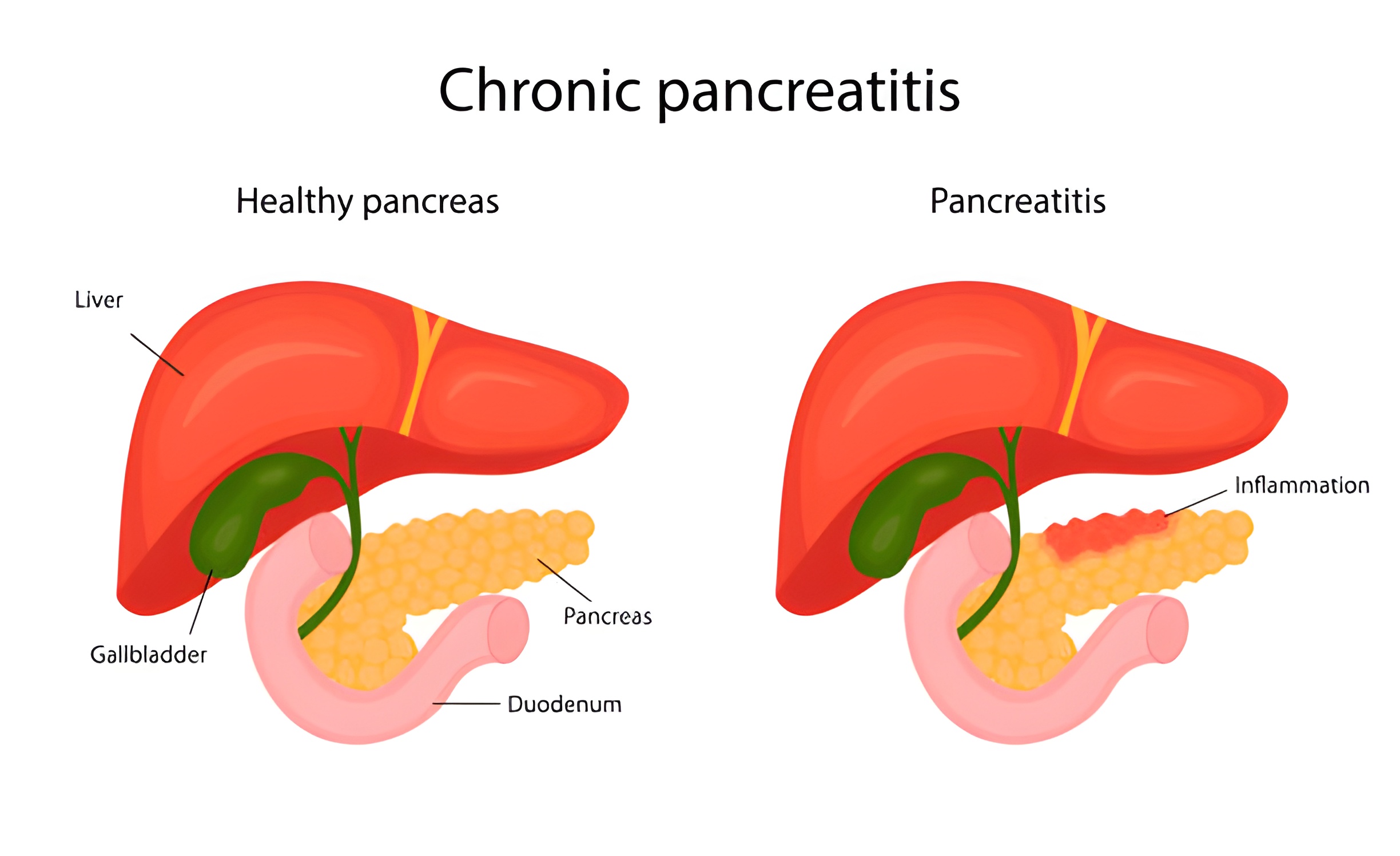
Symptoms of chronic pancreatitis
- abdominal pain: usually localized in the epigastrium and radiating to the back, increasing after eating and decreasing when sitting or bending forward
- nausea, vomiting
- diarrhea, steatorrhea (fatty feces), increased volume of feces
- bloating, rumbling in the stomach
- weight loss
- weakness, irritability, especially "on an empty stomach," sleep disorders, reduced efficiency
- red drops" symptom - bright red spots appearing on the skin of the chest, back, and abdomen.
If such symptoms occur, it is recommended to be examined to rule out chronic pancreatitis.
Symptoms of autoimmune pancreatitis
In many cases, autoimmune pancreatitis is asymptomatic or has mild symptoms, so people often go to the doctor when complications begin to develop. Symptoms of autoimmune pancreatitis include:
- slight pain or discomfort in the upper abdomen (especially after eating fatty or fried food);
- yellow skin and mucous membranes; digestive disorders (decreased appetite, dry mouth in the morning, nausea, flatulence, etc.);
- Diabetes mellitus; weight loss; increased fatigue;
- decreased ability to work; apathy, depressed mood (considered a manifestation of endocrine dysfunction of the pancreas);
- organ damage (development of renal failure, thickening of liver and lung tissues, etc.).
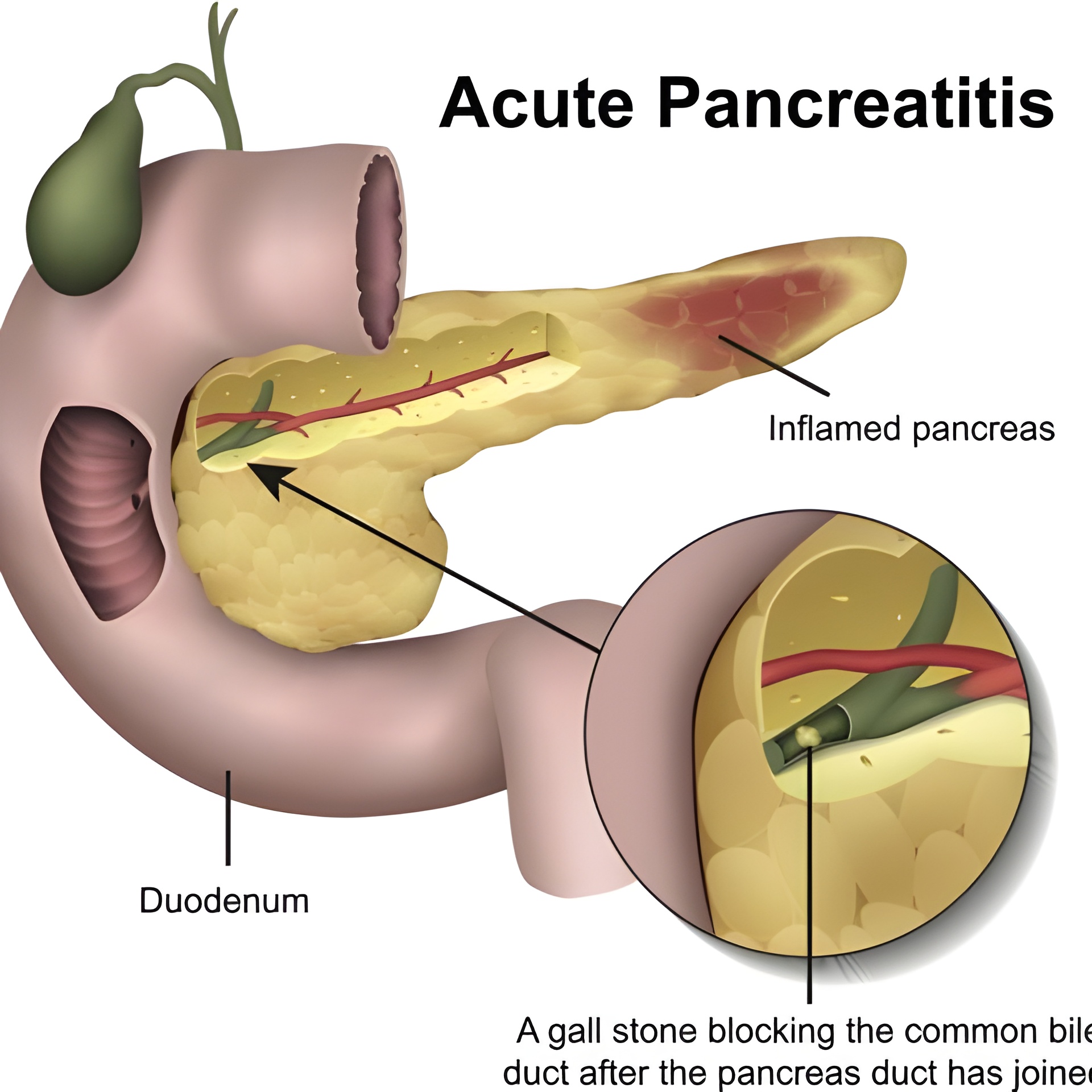
Symptoms of acute pancreatitis
- severe abdominal pain (in the area of the pancreas);
- nausea and vomiting;
- increase in temperature;
- tachycardia;
- rapid reduction of the patient's weight;
- flatulence;
- diarrhea;
- drop in blood pressure;
- white plaque on the tongue.
Acute pancreatitis is a severe condition, but it is quite difficult to diagnose.
Symptoms of alcoholic pancreatitis
As a rule, the first signs of pancreatitis in alcoholics begin with the onset of acute pain in the vivo, but they may extend to the back. They are also called shingles. These pains may occur suddenly, or they may be constant reminders. The patient gets worse after eating, especially fatty foods, smoking, or drinking alcohol.
Symptoms of alcoholic pancreatitis may include:
- diarrhea;
- flatulence;
- lack of appetite;
- nausea;
- vomiting;
- burp;
- bloating of the abdomen.
Gradually such consequences and complications of pancreatitis in alcoholics can develop:
- diabetes mellitus;
- pancreatic abscesses and cysts;
- jaundice;
- pancreatic tissue fibrosis or even cancer.
In addition, swollen and enlarged pancreas compresses other organs, which also leads to pain.
Diagnosis of pancreatitis
Laboratory methods:
- clinical, biochemical blood tests are performed (of particular importance are the levels of pancreatic enzymes in the blood - amylase, lipase)
- Co-program - the presence of certain substances (fats, soaps, fatty acids, etc.) in the feces is assessed. Normally they should be absent, but in chronic pancreatitis, due to insufficient production of enzymes by the gland to break down these substances remain undigested and are determined in the feces
- fecal elastase is an enzyme of the pancreas, the level of which decreases when it does not work enough
- in certain cases, it is important to identify cancer markers
- If there is a suspicion of hereditary genesis of the disease, a genetic study of the patient is performed.
Instrumental studies
- Ultrasound of the abdominal cavity. Signs of inflammation of pancreatic tissue, presence of stones in ducts, calcinates, cysts, gland tumors are evaluated. Additionally, changes in other organs of the gastrointestinal tract are determined to exclude complications of the disease, as well as concomitant pathology.
- Elastography of the pancreas. It allows determining whether there is fibrosis (thickening) of the pancreas, which is a criterion of the severity of structural changes in the organ.
Ultrasound with elastography of healthy pancreas
- FGDS. Visualization of the duodenum is necessary to assess the presence of inflammation in it, as well as indirect signs of pancreatitis. It is required to exclude inflammation and pathological formations (tumor, diverticulum) of the large duodenal nipple (through it the secret of the pancreas enters the duodenum, when it is blocked the outflow of this secret is disturbed, which leads to inflammation of the gland tissue).
Visualization of the stomach and esophagus is necessary to exclude erosions, ulcers, inflammation in them. Pathological changes in these organs are often combined with chronic pancreatitis, being mutually aggravating conditions.
- Additionally abdominal CT and MRI scans with cholangiography and RCCG may be prescribed. Necessary to confirm the diagnosis, as well as prescribed for suspected pathological masses in the pancreas, blockage of the gland ducts by a stone, tumor or cyst.
Treatment of different forms of pancreatitis
Treatment depends on the cause and symptoms of the disease, as well as the severity of the course. With this in mind, the doctor may prescribe:
- therapeutic hunger;
- the purpose of dietary nutrition;
- physiotherapy;
- medications.
MEDICAL DISCLAIMERThis content is for informational and educational purposes only. It is not intended to provide medical advice or to be a substitute for such advice or treatment by a personal physician. All readers of this material are advised to consult their own physicians or qualified health care professionals. UAmedTOURS is not responsible for the possible health consequences to any person or persons reading or following the information contained in this educational content. All readers of this content, especially those who take prescription or over-the-counter medications, should consult their physicians before making any changes in their diet, lifestyle, taking pills, or other facts that may affect your physical and psychological health.









